Prostate cancer is currently one of the most commonly diagnosed malignancies, accounting for approximately 20% of all newly diagnosed cancers. It is also the leading cause of cancer-related death among men (around 11%), having now surpassed lung cancer.
The disease is rarely diagnosed before the age of 40, while a clear increase in incidence and prevalence is observed with advancing age.
Risk factors associated with the development of prostate cancer include age, race, family history, diet, and long-term exposure to substances such as zinc and cadmium.
To date, the most well-documented risk factors are age and heredity, whereas the true contribution of the remaining factors has not been clearly established.In many cases, prostate cancer progresses slowly and may remain asymptomatic for years, while in other men it may be more aggressive. This is precisely why prevention and proper diagnostic evaluation are of paramount importance: the goal is to detect clinically significant cancer at an early stage—cancer that requires treatment—while at the same time avoiding unnecessary invasive procedures.
Prevention: What Every Man Should Know
Preventive evaluation typically begins with:
• PSA (Prostate-Specific Antigen): a blood test that may be elevated in prostate cancer, but also in benign conditions (e.g., benign prostatic hyperplasia, inflammation).
• Digital Rectal Examination (DRE) by a urologist, when deemed necessary.
• Risk assessment (age, family history, etc.).Modern clinical guidelines emphasize a more targeted diagnostic approach, as “blind” biopsy may miss significant lesions or detect small, low-risk abnormalities that might never cause harm (overdiagnosis/overtreatment).
What Is Multiparametric Prostate MRI (mpMRI)?
mpMRI is a specialized MRI examination that combines:
• High-resolution anatomical imaging (primarily T2-weighted images),
• Functional diffusion-weighted imaging (DWI/ADC): reveals areas where water molecule movement is restricted, often an indicator of malignancy. Suspicious lesions frequently demonstrate diffusion restriction, which may correlate with more aggressive disease,
• Dynamic contrast-enhanced imaging (DCE) with gadolinium in many protocols: highlights tissue perfusion patterns. Cancerous tissue typically shows increased angiogenesis.There is also the concept of biparametric MRI (bpMRI) (without contrast) in selected protocols, as contrast enhancement plays a more limited role in PI-RADS categorization and is not always necessary when the core sequences are of excellent quality.
PI-RADS: Why You See a “Score” in the Report
mpMRI findings are described using an international reporting system, PI-RADS (v2.1). Each suspicious area is scored from 1 to 5:
• 1–2: low probability of clinically significant cancer
• 3: intermediate / equivocal probability
• 4–5: high / very high probabilityThis score helps the urologist determine the next steps (surveillance, targeted biopsy, etc.).
When Is mpMRI Recommended and What Does the Patient Gain?
Based on current guidelines and clinical practice, mpMRI is often recommended:
• Before the first biopsy, when PSA levels or clinical findings raise suspicion,
• After a negative biopsy, when suspicion persists, as mpMRI can identify lesions that may have been missed by standard sampling.The benefits are practical and significant:
• Improved detection of clinically significant cancer: large studies show that mpMRI combined with targeted biopsy increases the detection of significant cancers compared with conventional random/systematic biopsy.
• Reduction of unnecessary biopsies in selected men: when mpMRI shows no suspicious lesion (PI-RADS 1–2), and depending on the individual risk profile, biopsy may be avoided or postponed under medical guidance (often in combination with markers such as PSA density).
• Targeted biopsy: when a suspicious lesion is present (PI-RADS ≥3), mpMRI guides the biopsy to the correct location, improving diagnostic accuracy.How the Examination Is Performed and What to Know Beforehand
The examination is painless and typically lasts 20–40 minutes (depending on the protocol). It is performed in an MRI scanner. Image quality is crucial: patient motion, rectal gas, or other factors may reduce diagnostic reliability. Therefore, structured preparation protocols (e.g., dietary instructions and, in some cases, measures to reduce bowel motion) help produce “cleaner” images and, consequently, higher diagnostic value.
Why It Matters to Perform mpMRI in an Organized Diagnostic Center
Prostate mpMRI is not “just another MRI.” It requires:
• an appropriate acquisition protocol,
• high image quality,
• radiologists experienced in PI-RADS assessment,
• and a clear, structured report that supports the treating urologist’s decision-making.The Examination at Euromedica Diagnostic Centers
At Euromedica diagnostic centers, multiparametric prostate MRI is performed using state-of-the-art high-technology MRI scanners, with specialized examination protocols, and is interpreted by experienced and specialized radiologists in accordance with internationally recognized diagnostic protocols and clinical guidelines.
Prevention, proper patient education, and the use of advanced imaging techniques can make a decisive difference in the management of prostate cancer.
Konstantinos Frigkas, MD Radiologist
Scientific Associate, Euromedica
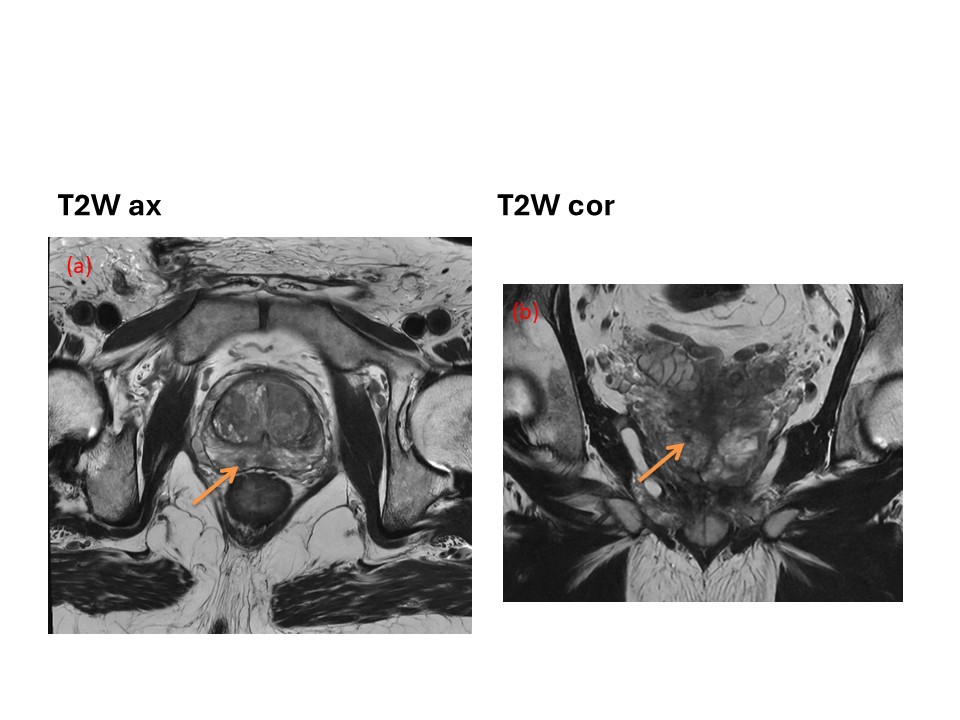
T2-weighted images in the axial (a) and coronal planes (b) demonstrate a small lesion (5 mm), of low signal intensity, located in the peripheral zone of the prostate gland (arrow), PI-RADS: 4.
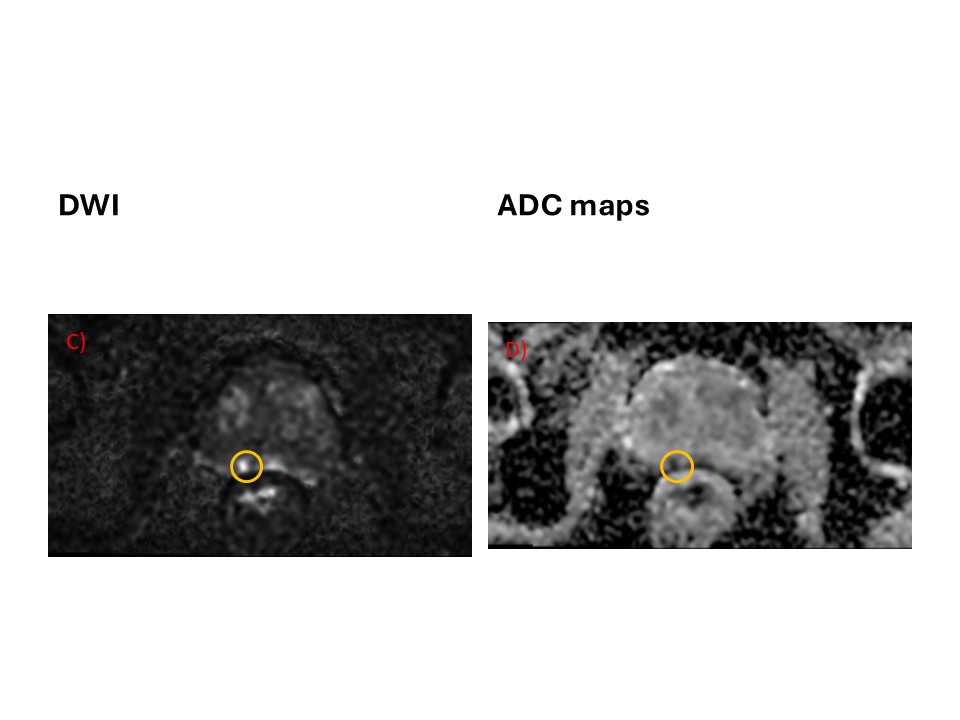
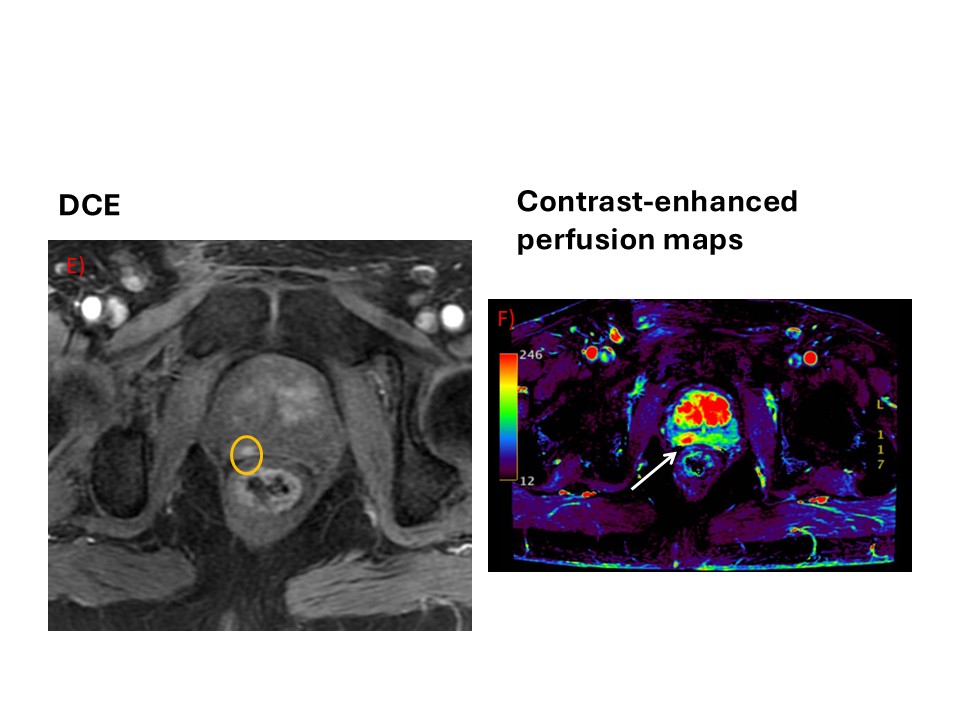
Final PI-RADS score: 4.
Radical prostatectomy: tumor with Gleason score 4+5, T2a, N0, M0.
